One Virus, Multiple Vaccines, Many Questions…
Humankind has dealt with deadly diseases and epidemics throughout its history. During the times when science and technology were still in their infancy, infectious diseases took many lives. In those days when even access to clean water was limited, let alone the lack of knowledge on hygiene, no drugs or preventive vaccines existed. Fortunately for humans, the world’s population was not as crowded as it is now, and long-distance travel was not as easy as it is today; otherwise the toll would probably be much more severe.
And as of now, for about a year, the entire world has been struggling with a pandemic again. A tiny virus even the naked eye cannot see has managed to fully take over the planet’s agenda. And finally, with the joint effort of many countries, we came closer to altering the balance in this struggle in our favour: the long-awaited vaccines are produced. However, new questions arose and we found ourselves in a confusing hail of disinformation.
How is the safety of a vaccine determined? Will these vaccines protect us for life? If we managed to develop a vaccine for COVID-19 within one year, why don’t we have vaccines for some diseases still? What do the mutations mean? Let’s address such important questions together, while providing vital basic information.
What kind of organisms are viruses?
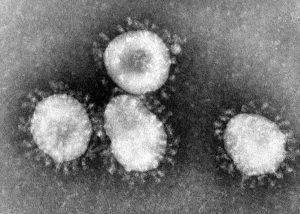
All living cells, by their nature, reproduce. They divide and pass on their genetic heritage, their genome, to subsequent generations. Viruses also carry genomes, which may be of either DNA or RNA structure. However, they lack the mechanism to copy these molecules and pass them on to new generations. For this reason, they enter other living cells, take them over, and have themselves copied by those cells. This is what we call an infection.
A virus cannot do anything unless it enters a living cell. It is merely an inert (or dormant) particle carrying a genome. The virus genome is surrounded by a protein shell called the “capsid”. Some viruses have an additional lipid covering called an “envelope”. The surface proteins of viruses bind to specific receptors on cellular membranes. A virus cannot enter a cell unless the cell has the desired receptors. Therefore, not every virus can infect every organism. Also, they cannot infect every cell in an organism, and thus the route of transmission varies accordingly.
For example, in order for the coronavirus that causes COVID-19 (SARS-CoV-2) to enter a cell, the cell’s membrane must have ACE2 receptors, and the knob-shaped proteins (Spike proteins) on the virus surface must bind to these receptors.
Viruses may differ in how they enter cells, and what they do once inside the cells, as well as how the infected organism reacts to an infection. Not every infection necessarily leads to disease. In fact, some viruses even benefit the organism they infect. However, if a large number of responses occur inside and outside the cell, or an immune response is generated involving many different cell types within the body, then the symptoms of disease begin to appear.
What are the deadliest infectious diseases caused by viruses?
Upon seeing the title, many of you may have thought of certain diseases: smallpox, flu, measles, rabies, Ebola, AIDS… All these diseases are lethal; rabies, for example, is almost 100% deadly once the symptoms begin to appear. Fortunately, protective vaccines are available for almost all of them. Smallpox vaccine, in particular, is special. Thanks to successful vaccination programs implemented worldwide, smallpox was declared “eradicated” in 1980, meaning this disease is no longer seen. On the other hand, a vaccine for HIV/AIDS has not yet been produced. But why?
Why can’t we produce vaccines for every virus easily?
The structure and behaviour of pathogenic viruses directly affect the effectiveness of both vaccines and drug treatments. In general, RNA viruses are more challenging. They mutate much easier and much faster than DNA viruses. This makes it difficult to produce effective vaccines and in some cases, requires reproducing vaccines at regular intervals. This is why seasonal flu vaccines are updated and reproduced every year or every 6 months.
Enveloped viruses follow a different strategy. New copies of viruses created inside the host cell borrow a piece of the host’s cellular membrane as their envelopes while exiting the cell. In other words, the envelopes of viruses copied inside the body are structurally similar to the host’s own cellular membrane. This way, they can protect themselves against the host’s immune system up to a certain stage. Plus, all they need to do to enter a new cell is to simply fuse their envelope with that cell’s membrane.
Retroviruses present an extra difficulty. Once these viruses enter a cell, they produce a piece of DNA from their own RNA genome and integrate this DNA into the host’s chromosomal DNA. Once infected, the cell cannot distinguish and separate the viral DNA from its own and carries on synthesizing the viral proteins throughout its life. If this cell divides, the same conditions are valid for all its daughter cells. One important reason why we still don’t have a licensed HIV vaccine until now is that HIV is also a retrovirus. Therefore, although AIDS patients can receive supportive treatment, their bodies cannot be fully cleared of the HIV infection.
What about other disease-makers?
Despite the presence of many useful, even indispensable bacteria, some bacteria species can cause deadly infectious diseases in humans. The most famous, perhaps, is the bubonic plague. Like smallpox and flu, this disease has appeared again and again at different times in different regions throughout history, causing many deaths. Thanks to correct hygiene practices and proper nutrition, it has been under control for a long time. A number of antibiotics have been developed, and they provide an easy treatment in most cases.
Apart from viruses and bacteria, viroids, protozoa, prions, some fungi, even some parasitic invertebrates, and insect larvae can also cause diseases in humans.

What is the purpose of vaccines, and how are they produced?
When the immune system detects a disease-causing organism, it responds to it. In addition to various cells produced by our immune systems as an initial response, the real strong response is producing antibodies against the pathogen’s antigens. The purpose of vaccines is to make sure that our bodies learn to produce antibodies against specific disease-causing pathogens, before their actual and active forms enter the body.
Vaccines contain a dead or weakened/inactivated form of the pathogen, and sometimes artificially created copies of some of its components. All vaccines that have ever been developed and applied are produced by one of these methods. Once the vaccine content enters the cells, their copies are manufactured inside the cells and are sent out. This triggers the immune response, and thus, the body “becomes acquainted with” the disease agent. Depending on the efficacy of the vaccine, the body retains this acquaintance for a certain period of time and knows what to do when confronted with the real deal.
What is an RNA vaccine? Is it a brand new technique?
In RNA vaccine technology, messenger RNA (mRNA) copies are used instead of dead or inactive virus fragments to create an immune response in the body. Regarding the COVID-19 vaccine, the mRNA fragments in the vaccine carry the code that enables the synthesis of viral surface antigens. These mRNAs, placed in oil droplets, are given to the cells via injection. Viral antigens are then synthesized inside the cells, and the immune response begins once these antigens exit the cells and are detected by the body.
The technique has been studied for over 20 years, and there are other vaccines previously developed with this technique (although their clinical trials are still ongoing). So, it’s definitely not a brand new technique, but surely a ground-breaking one. It enables producing a very large amount of vaccines in a very short time. Besides, the technique can be used to produce vaccines against other disease-causing organisms as well. Thanks to this technique, we are much better prepared for the next pandemic.
What do Phase 1, Phase 2, and Phase 3 mean?
It may take years to design, develop, and produce prototypes of therapeutic drugs and vaccines. Every drug or vaccine produced is investigated for their side effects and efficacy before being offered to common and extensive use. Some of this research is carried out on computers and/or in laboratories. All these stages constitute the “preclinical studies”. Experimental vaccines are also tested on animals to ensure they are safe and are effective at preventing diseases. The next step is to see the effects in the actual human body. Phase 1, 2 and 3 refer to the three-stages of “clinical trials” starting from this point on.
Clinical trials are subject to permission. No drugs or vaccines can proceed to the clinical trials without an approval by the related authorities. For safety and reliability reasons, trials start with a small number of participants and this number increases at each stage.
Phase 1: Conducted with a limited number of participants. The primary goal is to see if the vaccine is safe. Whether the vaccine induces an immune response and the proper dose of administration are also determined at this stage.
Phase 2: Conducted with hundreds of participants. The vaccine’s side effects and its success in generating an adequate immune response are closely monitored and reported. At this stage, a comparison is made on the vaccine’s effects, by giving a placebo to some of the participants instead of the actual vaccine.
Phase 3: The same study is repeated with the participation of thousands of people. The main output of the Phase 3 studies is the efficacy rate or effectiveness of the vaccine in preventing disease. The more participants there are, the more reliable the efficacy rate is. There is little concern about the serious side effects of a vaccine that has reached this stage, as the most common side effects would definitely be observed during earlier stages. Any vaccines observed to have caused severe or life-threatening side effects in a large number of people cannot reach this stage anyway. Exceptional cases can be seen, of course, but the same possibility is valid for even the simplest, over-the-counter drugs you use.
All stages of these trials are monitored and tracked by the relevant authorized institutions. Then, the entire data from all three stages are presented to the regulatory authority of the country where the vaccine will be manufactured and used, to apply for usage approval. Vaccines with efficacy rates above the value determined by these authorities and are proven to have very few serious side effects are approved. In emergencies such as a pandemic, approval for emergency use can be given. Mass production begins once all these steps are completed and all approvals are received. Vaccines go through a final quality control in each country where they will be administered.
How high should a vaccine’s efficacy rate be?
The highest efficacy rate currently known belongs to the vaccine developed to prevent measles: 97%. In other words, only 3 out of 100 vaccinated people are likely to develop the disease. The efficacy rate of seasonal flu vaccines, which are produced annually, is around 40-60%. The aim of the vaccine is not to prevent infection, but to prevent contracting the disease or to ensure that patients go through with symptoms as mild as possible. From this point of view, the efficacy rates of all the COVID-19 vaccines that are currently in use sll over the world are very good (and for most, it is above 90%).
How could it be possible to produce such effective vaccines in such a short time?
This is indeed the first time in the history of science that a vaccine could be produced this fast. Normally, all stages of vaccine production can take a long time -especially the pre-clinical stages. At this point, we need to remember that this is not the first time we have encountered a coronavirus. The same virus family greeted the world with SARS in 2002 and MERS in 2012, and thus, many studies were already initiated to combat these epidemics. This has helped the pre-clinical phases to be completed in just months (which would otherwise take 5 years or longer). Due to the pandemic, both the approval procedures and clinical trials were accelerated. While clinical trials may normally take 6-7 years, they were completed within months, and applications were immediately made to receive approval for emergency use. Meanwhile, vaccine companies also took the initiative and started mass production before applying for approval. This was a risk on their behalf because their vaccines might not have gotten an approval. But they did so anyway due to the urgency of the situation and the huge demand for vaccines from around the world. It is fortunate that they did so; this allowed the vaccines to be distributed around the world almost as soon as the approvals were given.
What about the mutations?
Mutations are changes in the nucleotide sequence of DNA or RNA molecules in an organism’s genome. Each time a DNA or RNA molecule is copied, there is a possibility for mutations to occur and a mutant copy to be formed. In every organism, at all times. Mutations can harm or benefit the organism, and they may sometimes be entirely ineffective. As the complexity levels of organisms increase, the number of mechanisms that control and/or mutations also increase. Viruses mutate much faster due to their structure.
Researchers constantly monitor mutations in pathogens. They closely observe if the prevalence of these mutations increase and if they cause any considerable differences in the virus. Mutations that increase in prevalence and have the potential to cause a change the course of the disease are monitored much more closely, and additional measures are taken to control the spread of these mutations when necessary.
Scientists recently detected a mutation that is thought to cause SARS-CoV-2 to spread more rapidly, and as an additional measure, quarantine practices were tightened in regions where this mutation is seen. These mutations are not expected to reduce the effectiveness of vaccines that are in use (for now) as the vaccines trigger a broad, multifaceted immune response. However, if otherwise, available vaccines can be altered and updated accordingly within a short time.
Back to the new coronavirus …
The coronavirus that causes COVID-19, namely SARS-CoV-2, is an enveloped RNA virus. It targets epithelial cells that have ACE2 receptors on their surface. After invading these cells, it forces them to produce both its RNA molecule and structural proteins. The newly manufactured coronaviruses exit the cell by “enveloping” themselves with the membranes of epithelial cells, and they begin to chase new cells to infect. When the infection reaches a certain level, our immune system is activated and the disease symptoms begin. The overreaction of the immune system can cause severe symptoms, which then requires a tough treatment.
SARS-CoV-2 is both very contagious and can remain in the body for a long time without giving any symptoms. Because of these two features, the toll is quite heavy. Still unaware that you are infected, you can transmit the virus to a large number of people. We cannot foresee in everyone how severe the course of the disease will be, and unfortunately, there are currently no drugs yielding wonderful results in a short time in severe cases. We use the ones we already have, and depending on reports regarding their effects, we either continue to use them or move on to another drug candidate.
Yes, the follow-up process of Phase 3 clinical trials of vaccines is still ongoing. Yes, we do not yet have enough data on the long-term effects of vaccines in different age groups. But we don’t have enough time to wait for these data either. The burden on healthcare systems is clear. All of the vaccines have been produced with the techniques that have gone through enough trial and error, and are products of a background fed with many years of knowledge and technological advances. The most logical option we have is to proceed by following a profit and loss account. It is up to us how this will result and how quickly we will reach that point. Global impact with individual measures.
REFERENCES
- 1. https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- 2. https://www.who.int/news-room/q-a-detail/vaccines-and-immunization-what-is-vaccination
- 3. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/index.html
- 4. https://www.niaid.nih.gov/research/vaccine-types
- 5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6777997/
- 6. https://www.ncbi.nlm.nih.gov/books/NBK21523/
- 7. https://www.medicalnewstoday.com/articles/158179
- 8. https://www.medicalnewstoday.com/articles/what-is-vaccine-efficacy
- 9. https://www.britannica.com/science/virus
