A Novel Approach for Treating Cancers: Immunotherapy
Cancer is a hard reality. It still remains one of the greatest health challenges of humanity and a leading cause of death worldwide. According to the World Health Organization (WHO), cancer accounted for nearly one in six deaths in 2020.
Cancer rates may have spiked significantly in recent years due to the effects of modern carcinogens and industrial pollutants, but the incidence of cancer in the pre-industrial world was not too low either. In fact, a 2021 study reported that the cancer rate among people living in medieval Britain was approximately 25% as common as it is today. People at those times were also exposed to carcinogens, including solar radiation and pollutants (although pollutants were mostly in homes and other indoor environments). Besides, they were more vulnerable to viruses and other pathogens and didn’t have access to proper diagnosing methods or therapies.
However, the introduction of modern-day carcinogens such as tobacco and industrial pollutants made a big difference. The increase in population and life expectancy also played a part in this difference. Even though today’s risk factors also include unhealthy dietary habits and lack of physical inactivity, pollution and smoking continue to be the top risk factors especially in developing countries, where they account for an 81% to 100% increase in respiratory cancers.
Cancer, as we know, is in fact a generic term for a large group of diseases. Characterised by a rapid and seemingly uncontrolled proliferation of abnormal cells in any part of the body, over a 100 different types of cancer are currently known to affect humans. Another defining feature of cancer is its ability to spread to other tissues (metastasis) –which usually is the primary cause of death from cancer.
Depending on how far cancer has spread and progressed at the time of diagnosis, different methods can be used for treatment. The most common are surgery, chemotherapy, and radiotherapy. Surgery is the primary method of treatment if the cancer is localised and isolated, but it is not suitable or efficient for some cancer types. Chemotherapy relies on agents designed to kill cells that divide rapidly, but its toxicity to other tissues in the body poses a great concern. Radiation therapy, or radiotherapy uses ionizing radiation to damage the DNA of cancerous cells, and is a bit more “target-oriented”. However, there is always the possibility of damaging healthy tissues near or around the targeted tumour.
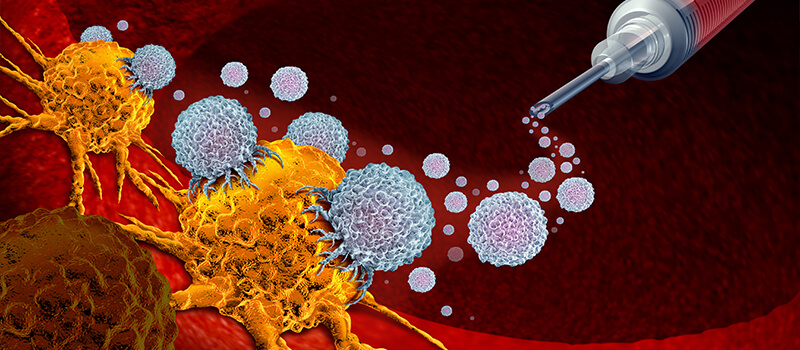
Some cancers can also be treated with bone marrow or stem cell transplantation, while some are suitable for “targeted therapies”, which use drugs that target molecules specific to cancer cells. And now another option exists: immunotherapy. This method, unlike any other, uses the body’s own defence mechanism to combat cancer. In summary; it stimulates and encourages the immune system to find and destroy cancerous cells. Despite being relatively new, the list of its success stories has been growing rapidly.
For now, immunotherapy is used for many types of cancer, and its efficacy increases by around 20–30% when combined with conventional treatment methods. Of course, it is not side-effect free. Adverse effects can be seen if the body creates an excessively strong immune response. However, with close communication between the patients and medical specialists, it is possible to successfully manage these side effects. Despite the risk, immunotherapy has revolutionized the way we treat cancer and has fundamentally changed our view of how cancer can be managed, especially in patients with advanced cancer.
Unleashing the immune system
Towards the end of the 19th century, scientists began to focus on the idea of activating the immune system as an alternative -and possibly safer- strategy for attacking tumour cells. As the concept drew more and more attention, a growing number of scientists rolled up their sleeves to dive deeper into research. In the 1990s, James P. Allison and Tasuku Honjo independently studied proteins that operate as “brakes” on the immune system. They set out with the idea of finding a way to inhibit these breaks, which would unleash the immune system to find and destroy tumours. They worked on different strategies and obtained spectacular results, which brought them the Nobel Prize in Physiology or Medicine in 2018. And thus, a novel method for cancer treatment emerged.
Why does the immune system have breaks?
Our immune system fundamentally has the ability to discriminate “self” from “non-self”. Think of it as guards constantly patrolling the body, looking out for intruders or invaders. Once an intruder is detected, certain white blood cells (particularly T-cells) are encouraged to bind to them, calling the immune system to engage in defence.
Some proteins act as T-cell accelerators, and when they get involved, the body gives a full-blown immune response. In some cases, this response may be too strong, depleting the body’s resources and even leading to the autoimmune destruction of healthy cells. To prevent this, a second mechanism exists: immune activation inhibitors, or “the breaks”. There is an intricate balance between these accelerators and brakes, which ensures that the immune system effectively combats invaders but does not give an excessive immune response that may further damage the body.
How does immunotherapy work?
Cancer cells have specific molecules on their outer surfaces, called “tumour antigens”. Antibodies of the immune system can detect and bind to these abnormal antigens. However, cancer cells are masters of disguise, evading the immune system with several strategies in most cases. Immunotherapy helps the body to find them. Different types of immunotherapy do this in different ways.
The most common type of immunotherapy is “immune checkpoint” therapy. It targets the brakes, which act as checkpoints in creating the desired immune response, to enable the body to respond more strongly to cancer. Scientists are now working on finding additional checkpoint proteins because combinations of different agents (just like in chemotherapy) have been shown to work better.
Another widely used method utilizes “monoclonal antibodies”, which are slightly modified antibodies. Not only do they find and bind to tumour antigens, but they also mark them —in a sense, they also plant a red flag for the immune system. This drives and helps the body’s own defenders to find all flagged cells and destroy them.
One type of immunotherapy that is still in the experimental stage is the T-cell transfer, also known as “active immunotherapy”. For this purpose, immune cells around the tumour are collected, and the most active ones are selected and reproduced in the laboratory, re-trained, and given back to the body. The aim is to increase the natural combat ability of T-cells, the soldiers of the immune system.
Another method uses a number of different active agents, called immunomodulators (interleukins, cytokines, interferons, chemokines, and immunomodulatory imide drugs -IMiDs). The aim here is, again, to enhance the body’s immune response. Their composition and structure can be natural, synthetic, or recombinant. Some of these molecules affect certain parts of the immune system, while some have a more general effect. At this point, it is worth mentioning that the BCG vaccine and COVID vaccines also rely on immunomodulators. This is why the BCG vaccine is also useful in the treatment of bladder cancer.
Is immunotherapy used for other purposes?
Yes. Besides being used for amplifying a person’s immune response in cancer treatment, some immunotherapies are designed to reduce or suppress the immune response. These are especially useful to stop the body from attacking its own cells or organs in autoimmune diseases or to help the body accept a foreign tissue in organ transplantation. Plus, they provide an additional advantage by helping the body build an immune tolerance, which means that the patients do not have to be dependent on immunosuppressive drugs for life. Of course, this also eliminates the risk of potential side effects of these drugs. Immunotherapy can also be used to treat allergies, to reduce sensitivity to allergens.
Assoc. Professor Gülcan Bulut from Medicana Hospital in İzmir is a young Medical Oncologist, who has been working with immunotherapy applications for six years. This is exactly the time when applications started to become widespread in Türkiye. She answered our questions about immunotherapy
What is the current situation of immunotherapy studies and applications in Turkey?
Until 5-6 years ago, we were only able to reach immunotherapy through Phase-3 studies. Now we have come to practice it in our routine clinics. We are not dependent on other countries. Drugs can be obtained from pharmacies in Türkiye with a prescription. Patients can now receive immunotherapy in any place where there is a chemotherapy unit and an oncologist. The number of our experts is also increasing. The only requirement is that the disease should have an indication from the Ministry of Health (that is, a certain type of immunotherapy must be approved for that given disease). However, whether the drug will be reimbursed depends on the health insurance.
As for clinical trials, immunotherapy drug trials continue in about 10-20 centres, and patients are still referred to these centres for many types of cancer. These are tertiary care hospitals, places that can do these studies. There is also access to immunotherapy within the scope of clinical trials.
 How do you decide on using immunotherapy for a patient?
How do you decide on using immunotherapy for a patient?
We define the tumours as cold or hot, depending on their antigen-forming capacity. The more antigens a tumour has, the hotter it is. For example, melanoma is a hot tumour. In such hot tumour types, if a Phase-3 study has been conducted and shown to contribute to the patient’s condition, then we decide to apply immunotherapy. The most commonly available and widely used ones are immune checkpoint drugs. These drugs, known as Anti PDL-1, Anti PD1, and Anti CTLA, are either used alone or in combination. All drugs we use must be approved by the Ministry of Health. Before deciding on a drug, your physician may ask you for molecular pathological staining. Sometimes, we use immunotherapy as a maintenance treatment after the patient’s chemotherapy and/or radiotherapy is finished.
Are these therapies suitable for all cancer types?
What’s important here is the type of cancer cell and the characteristics of the tumour. We were first introduced to immunotherapy in cases of melanoma and renal cell carcinoma. Later, it started to be used in the treatment of many cancers such as lung, head and neck, stomach, colon, and cervix. In certain types of lung cancer, we got results far, far above our expectations. Studies continue with all cancer types. However, apart from clinical studies, we are currently only able to use these drugs in cancers for which their effectiveness has been proven. We predict that these drugs will come into use at least in some stage of all cancers, except for a few types, if not all.
What are the most common adverse effects?
We cannot compare the side effects of immunotherapy with chemotherapy, because these drugs have different side effects. We generally see side effects such as skin rashes or itching, diarrhoea, and sometimes deterioration in endocrine tests (hormone levels) due to the over-activation of the immune system. However, not all of these are seen in the same patient. The most common side effect we encounter is an increased activity of the thyroid gland. However, these side effects are at very low rates, and they are all easily managed.
“As we get to know cancer more, our treatment options increase,” says Assoc. Prof. Dr. Bulut, and adds, “The genome atlas project provided a very serious acceleration because after mapping the human genome, the tumour genome was also mapped. We are now able to see what genetic changes have occurred in tumour development, and studies continue on developing drugs targeting genetic changes.” Finally, she sums up what an exciting path we are now on: “Immunotherapy has completely changed the scheme ahead, it changes the conventional treatment algorithms.”
REFERENCES
- 1. https://www.cancerresearch.org/what-is-immunotherapy
- 2. https://www.cancer.gov/about-cancer/treatment/types/immunotherapy
- 3. https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/immunotherapy.html
- 4. https://www.who.int/news-room/fact-sheets/detail/cancer
- 5. https://www.nobelprize.org/prizes/medicine/2018/press-release/
