How Would You Like Your Cell Sheet?
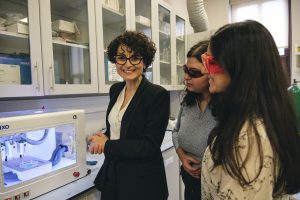
Prof. Seda Kızılel from Koç University’s Department of Chemical and Biological Engineering and her team won the first prize in the Health and Life Sciences category at TEKNOFEST 2023 with their pioneering work on cell sheets and their revolutionary project on live tissue repair. Prof. Kızılel told KURIOUS about the challenging process that led them to this important discovery.
Imagine a thin sheet, akin to a band-aid, crafted from your own cells. When applied to a damaged tissue in your body, it is able to repair it using your cells. Although it may sound like a product of science fiction, these cell sheets have been deployed in clinic use for the past 4-5 years to repair damaged or dysfunctional living tissues. They find particular use in tissues of the heart, lungs, cartilage, and cornea (the outermost layer of your eye). Yet, their most pivotal application undoubtedly lies in repairing nerve tissue.
Nerve cells divide at a sluggish pace. Consequently, other cell types in the surrounding tissues proliferate more rapidly, filling the damaged area before nerve cells can. As the self-healing capacity of nerve tissue is severely restricted due to this phenomenon, cell sheets emerge as a potentially life-saving technology for repairing nerve tissue damage.
Let’s delve into the production process of these sheets: Healthy cells are harvested from the person’s damaged tissue via biopsy. These cells are then cultivated in the laboratory through specialised techniques, allowing them to proliferate and form cell sheets as they align closely together. Think of them as “personalised” tissue patches. Since the cells originate from the patient, there is no risk of tissue rejection. In some instances, they can be multi-layered, with layers consisting of different cell types that match the structure of the target organ. For instance, the heart comprises dense muscle tissue covered with a thin layer of epithelial tissue. A cell sheet designed for the heart would mirror this multi-layered structure —muscle cells at the base with epithelial cells on top. These sheets do not nourish the underlying tissue; instead, they serve as a direct patch: Covering the damaged area with healthy cells, where they ultimately heal the tissue and repair the organ.
This technology is particularly crucial for medical conditions like spinal cord injuries, where tissue self-repair is challenging and even limited. As expected, the market demand for such products exhibits a growing trend. In the next decade, the market for smart cell culture plates is anticipated to reach around three billion dollars, though substantial investment support is necessary for large-scale production.
For their pioneering work on these cell sheets, Prof. Dr. Seda Kızılel from Koç University’s Department of Chemical and Biological Engineering, along with her team comprising Dr. Kiyumars Jalili, Ph.D student Esra Yalçın Kaya, and Işılay Göktan, received the “Best Initiative” prize in the Health and Life Sciences category at TEKNOFEST 2023. This innovative product stands as a striking example of the fruitful integration of biology, chemistry, and technology.
Dr. Kızılel’s personal journey also adds a poignant dimension to the narrative. A few months after filing a patent application for their work, Dr. Kızılel underwent an oesophageal surgery. A few weeks post-operation, she received a call and learned that their application was accepted, and their patent even won an award. In that moment, Dr. Kızılel thought of the potential application of their cell sheets in oesophageal repair. Unfortunately, since this realisation came after the surgery, Dr. Kızılel missed the opportunity to benefit from her own invention.
How did you feel when this happened?
The timing was quite intriguing. I had lesions in my oesophagus due to anaemia, a common condition among women. When this is uncorrected for a long time, it leads to the dysfunction of some enzymes in the larynx and may result in the formation of a specific tissue called Plummer-Vinson, which unfortunately has the potential to form lesions in time. This tissue was surgically removed. Following the procedure, as the inner lining of the oesophagus was healing, it narrows due to scar tissue and oedema formation, causing difficulties in swallowing for 8-9 months. This necessitated medical intervention several times, where oesophagus was endoscopically cut. Had there been the opportunity to use these cell sheets immediately after tissue scraping during surgery, I wouldn’t have suffered these problems. Unfortunately, it was too late for me. However, using cell sheets produced from the patient’s own cells may prevent other people undergoing oesophageal surgery from facing the problem of laryngeal narrowing. To be honest, I hadn’t even considered oesophageal application until that moment. Our initial focus was on spinal cord injuries due to the significant need in that area. Surprisingly, applying the same technology in the oesophagus is easier than the nerve tissue.
Are there other examples of your work in the world?
Yes, there are other research groups working on similar products. For instance, a group in Japan produces cell sheets using oral mucosa cells, and their product is currently the only one on the market. However, they employ a complex technique that is already patented, which comes with certain limitations. As they work in room temperature, the viability of cells and the integrity of sheets can be damaged, at least partially. They only work with single layers and have no data on neural tissue applications.
What is the superiority of your cell sheets?
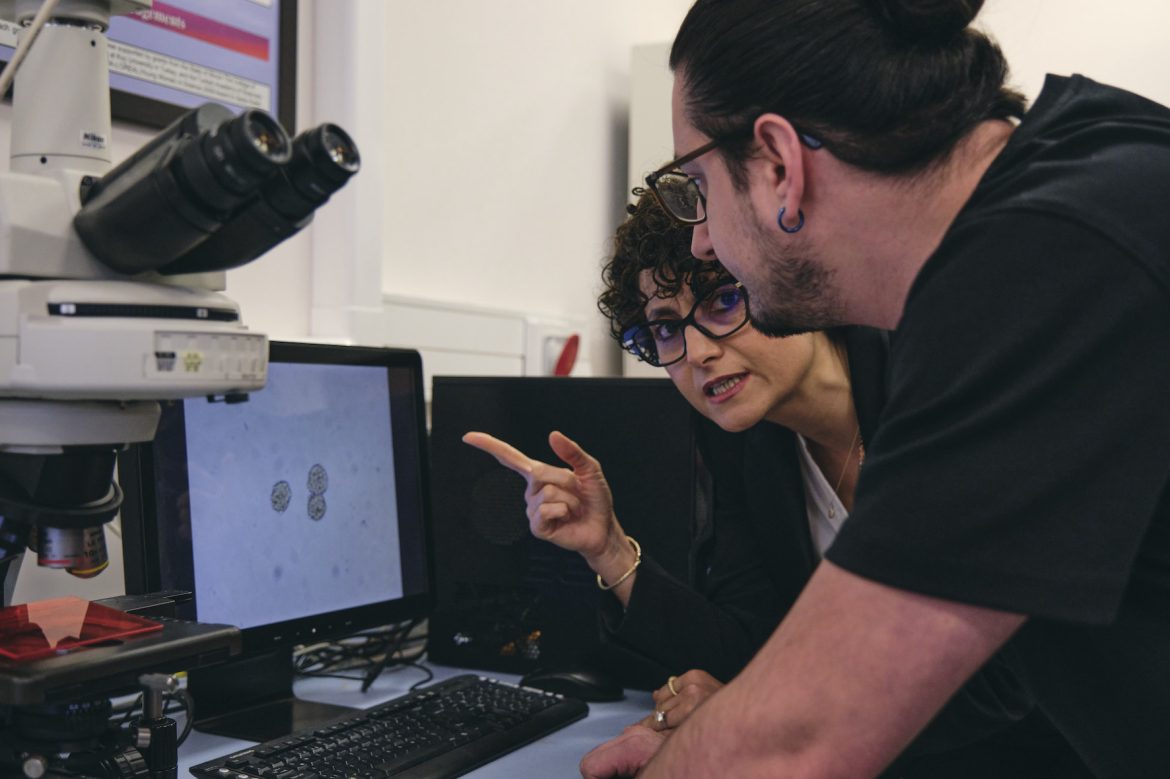
The technique we employ is more efficient and faster. Producing the cell sheet is just the beginning, separating the sheet from the surface it is grown on is one of the crucial aspects. During this process, you have to ensure the cells remain viable and the integrity of the sheet stays intact. We have overcome this challenge by manipulating the chemistry of the growing surface, with a temperature sensitive surface design. This enabled us to to replicate the cells preserving their viability and function, and separate them from the surface without disrupting the integrity of the sheet, with higher efficiency compared to existing samples on the market. Compared to existing applications, we are able to produce cell sheets with higher efficiency of forming multilayered plates, and with total control on the thickness of the surface chemistry. We have experimented with various cell types, including nerve cells, and most importantly, our production technique comes at a much lower cost. However, these are merely laboratory results. We need to scale things up to validate our data, so that the work does not remain in the laboratory. For this to happen, we need an investor to support this project.
What if it cannot be scaled up? Will the project be shelved as it is?
Unfortunately, that is what will happen unless we are able to validate our laboratory data. Unfortunately, this happens very often. In a study we published in 2015, we had managed to integrate a polymer into the asphalt we developed, and by also integrating salt into this polymer using nanoparticles, we were able to delay freezing by 27 minutes. However, this project did remain in the laboratory as the company we worked with did not conduct trials on the pilot scale. When laboratory results cannot be verified on a larger scale, you are left with the technology you developed, withouıt being able to implement it in real applications.
Can we get some technical details for KURIOUS readers? How do you produce the sheets and how do you separate them?
To keep the cells alive, we produce them at 37 degrees Celsius. We use a temperature-sensitive polymer on the surface. First we seed the cells on these polymer and wait for the cells to grow and come together, forming a layer. When the medium temperature decreases by 5-7 degrees, the polymer on the surface shows conformational properties (reversible change) and releases the cell layer.

If large-scale production can be achieved, will the system be the same?
Yes, the system will remain largely unchanged. However, all steps must be conducted in ultra-sterile conditions, where even air particles are monitored, and everyone wears specialised clothing. The final product must maintain this ultra-sterility, especially if intended for surgical use. Meaning, if a surgeon is to use it, the product must remain ultra-sterile until the package is opened during an operation. All of these aspects, particularly the production units required, contribute to increased costs. This is essentially the reason why we need investors.
Is it also possible to produce stem cell sheets that can differentiate into any cell type? Would that be easier?
Indeed, it is possible to produce stem cell sheets. However, there are different types of stem cells, and your selection of stem cells must correspond to the tissue you intend to generate. Also, you will need different conditions and different molecules based on the type of tissue these stem cells are meant to develop into. Consequently, this process may incur slightly higher costs. However, harvesting the patient’s own healthy cells via biopsy would give you cell sheets faster and in a more efficient fashion.
What could be the next step? For example, could it be possible to deliver drugs to the damaged tissue?

One of the projects we are currently working on already includes this design. We will incorporate nanoparticles onto the top layer of a multi-layered plate, and load these nanoparticles with drugs to facilitate targeted drug delivery to the tissue to be repaired.
We hope to see the production of these remarkable cell sheets and plates, currently manufactured by only one company globally, within our own country. By doing so, we may offer unparalleled medical support to numerous individuals. This pioneering technology, particularly in the treatment of spinal cord injuries, has the potential to elevate our country to a more powerful position in the realm of science. We extend our gratitude once again to Dr. Seda Kızılel for her invaluable contributions.
